Orthopaedics

September 2, 2025
CRMC Earns Blue Distinction Center Status in Knee and Hip Care
For the seventh year in a row, Cuyuna Regional Medical Center (CRMC) has been recognized as a Blue Distinction® Center for its Knee and Hip Replacement programs.
August 1, 2025
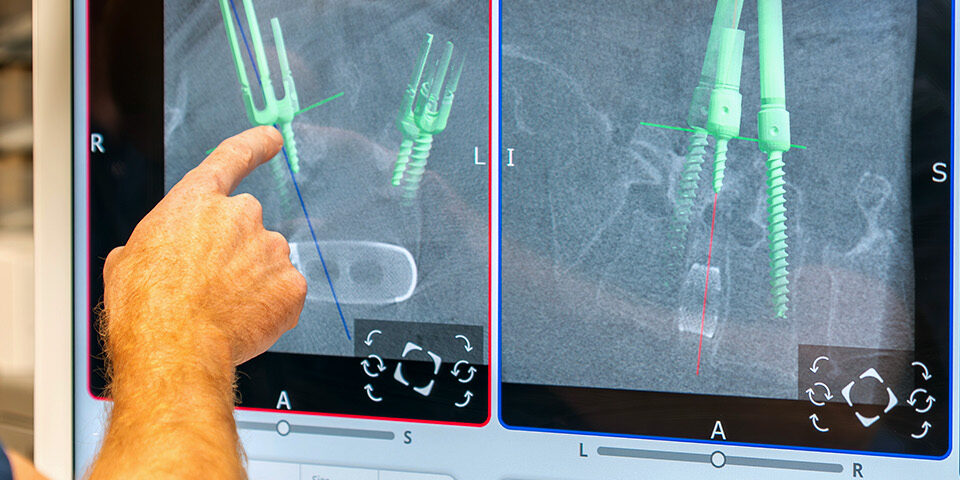
CRMC Leads the Way in Assisted Robotic Spine Surgery
CRMC now offers the VELYS™ Active Robotic Assistance Platform (VELYS™ Spine), a cutting-edge system with active robotics that automatically adjusts to patient movement and challenges during surgery. It’s designed to enhance precision across a variety of complex back and neck procedures.

May 29, 2025
When Lifting Your Baby Hurts: What to Know About Mommy’s Wrist
Learn about De Quervain’s Tenosynovitis, or “Mommy’s Wrist,” and explore treatment options for postpartum wrist and thumb pain.

March 3, 2025
Innovation: Orthopaedic Team Contributes to Robotic Surgery Study

February 20, 2025
Spine Clinic Expands to Baxter
The Orthopaedic Spine Clinic expands to Baxter.

September 16, 2024
CRMC to Present on Unique Hand Therapy Treatment at National Conference
Cuyuna Regional Medical Center (CRMC) proudly announces that Rose Bankers, OTR, L CHT, will present at the American Society of Hand Therapists Annual Meeting in St. Louis, MO. This is the first time someone from CRMC or regionally has presented at the four-day conference, which shines a spotlight on innovations in hand therapy. CRMC is one of 47 presenters from across the nation, making it a significant achievement.

July 1, 2024
Cuyuna Regional Medical Center Earns AAHKS Fellowship Recognition
Fellows beginning their training this summer at CRMC will be the first class graduating from an AAHKS-Recognized program.

June 27, 2024
New Podiatrist Joins Orthopaedic Department
Stephen C. Schmid, DPM, FACFAS, joined the medical staff at Cuyuna Regional Medical Center (CRMC), in July 2024 as a Podiatrist. He will diagnose and treat people with a range of foot and ankle conditions, from routine checkups to reconstructive surgery.

May 6, 2024
Comprehensive Orthopaedic Care in Lake Country
Whether it’s a sports injury, joint pain, or any other orthopaedic concern, our expert team will personalize a plan to address your needs and get you back to doing what you love.

May 3, 2024

