Living in the Shadow: A Story of Survival, Trauma, and Healing
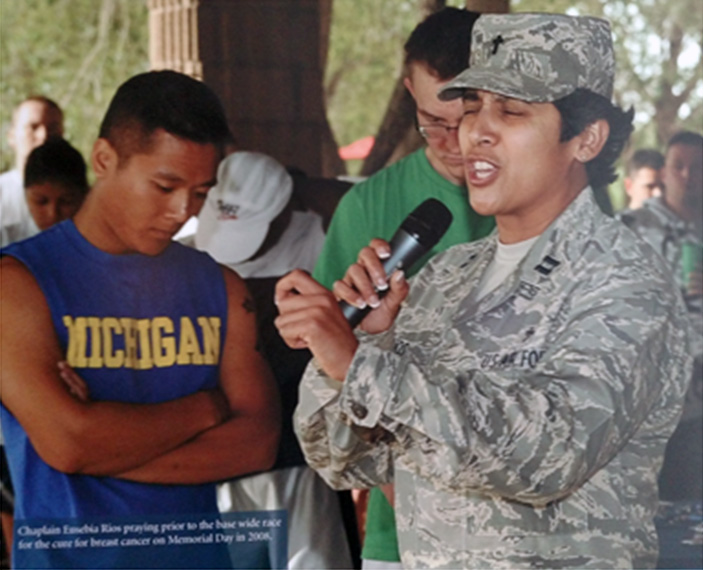
By Chaplain, Major (Ret.) Eusebia Rios
Chaplain Rios served 33 years in the U.S. Air Force, managing the Air Force Chaplain Candidate Program and deploying 18 times.
“What a beautiful day.”
The sun was shining. Birds were literally singing outside the window. It was the perfect start to a gorgeous morning. She sat down to admire the deer grazing peacefully just ten feet from the patio. It was undoubtedly the beginning of something good.
Then, as she bent down to tie her shoe, it happened.
She calls it “the shadow.”
In an instant—with her shoes still untied—her body stiffened, her posture straightened, and her senses went on high alert. The room suddenly felt vacant. The bright view outside turned grey. Dread flooded her body. Adrenaline surged through her legs. Every muscle was filled with blood and tension. Sweat gathered on her brow. She clenched her fists. She was ready to fight.
Everything else disappeared, except the primal instinct to survive.
She became hyper-aware of every sound.
Her heart pounded in her chest.
She could hear her own breathing.
In that moment, she told herself, “You’ve been here before.”
She recalled the feeling from standing outside a car accident rescue… from holding the hand of a fallen battle buddy… from the moments before a gunshot… from the split second before she had to run to safety… from the countless times she prepared to fight for her life.
“You know this feeling,” she whispered to herself. “Now remember where you are.”
She took slow, deep breaths.
She reached down and touched the cushion beneath her, focusing on its texture.
She opened and closed her fist.
She closed her eyes and recalled the beauty of the morning she had just witnessed.
Then she repeated, like a mantra: “You are home. You are safe. You are tying your shoe. You do not have to fight to get to your car. You are okay. You can let the fear go. You are not powerless. You are okay.”
Gradually, a sense of calm wrapped around her like a blanket. The pressure eased. Time, once warped, returned to normal. What felt like thirty minutes had only been a few.
As she sat recovering from the episode, she allowed herself to soak in the feeling of being okay—a feeling she had fought so hard to reclaim.
She remembered the nights she avoided sleep, afraid to relive traumatic scenes.
She remembered people asking, “What’s wrong?” and her replying, “Nothing,” while thinking to herself, “I don’t know.”
She remembered how a scent could trigger a memory of a traumatic event.
She remembered the dreams that left her helpless.
The fear she had locked away to stay mission-ready.
The day that fear broke loose and flooded her life, paralyzing her emotionally, mentally, and physically.
She remembered how she would snap in frustration over minor things.
How her loved ones reacted with concern—concern she rejected because she didn’t want to admit the truth.
She remembered asking herself, again and again, “What’s wrong with me?” and still not knowing the answer.
She remembered the day she finally asked for help, and how she wished she had done it sooner.
She had been raised in a culture of resilience, told to “tough it out,” to press on.
She was told: “You don’t need to deal with that—it’s just part of the job. Get over it, or people will think you’re not cut out for this.”
But counseling gave her a safe place to start unpacking what she had carried for years.
She realized she was one of the lucky ones.
Some of her friends turned to alcohol to numb the pain.
Some ate their way through trauma.
Others ran themselves into exhaustion just to fall asleep at night.
Many disconnected from friends and family, some lost in isolation, some lost entirely to suicide.
The Broader Truth
Not all Post Traumatic Stress Disorder comes from combat or emergency scenes.
Anyone who has witnessed death, trauma, or a life-altering event can experience deep psychological and emotional wounds.
Asking for help before the breaking point is ideal. But too many of us believe we’re stronger for “pushing through.”
Unresolved grief, witnessing death, caregiving through chronic illness, supporting the grieving, pouring out compassion daily – these are all soul-draining experiences.
Even the loss of a beloved pet can open deep wounds.
When the things we’ve “tucked away” finally come crashing down, we may find ourselves emotionally, mentally, and spiritually in quicksand.
Please, remember you are not alone.
Reach out to the social worker.
Reach out to mental health professionals.
Reach out to the chaplain.
Reach out.
If Minnesota weather has taught us anything, it’s that we can’t always predict when or where a storm will hit. But we can prepare. We can support each other. We can process the weight of this work, together.
So check in with each other.
Let others ask you, “Are you okay?”
Be honest with yourself.
And know this: You are loved. You are supported. You are valued by your entire CRMC medical team.
PTSD Statistics
How common is PTSD?
Nearly 4% of the global population had PTSD at some point in their lives. (World Health Organization, 2024)
Of the 70% of people who experience a potentially traumatic event, about 5.6% develop PTSD. (WHO, 2024)
In the U.S., the lifetime prevalence of PTSD is 10-12% for women and 5-6% for men. (American Psychological Association, 2024)
U.S. PTSD statistics:
About 9 million Americans are affected by PTSD. (National Alliance on Mental Health, 2024)
About 37% of Americans with PTSD have severe symptoms. (NAMI, 2024)
About 6% of Americans will have PTSD at some point in their lives. (NIMH, 2023)
About 7% of U.S. veterans will have PTSD at some point. (National Center for PTSD, 2024)
As is true in the global population, U.S. women are significantly more likely than men to experience PTSD. (NAMI, 2024)
The following statistics from the report illustrate the percentage of these traumatic experiences that result in the person receiving a PTSD diagnosis:
- Rape: 19.0%
- Physical abuse by romantic partner (now called intimate partner violence): 11.7%
- Kidnapping: 11%
- Sexual assault (other than rape): 10.5%
- Being stalked: 7.6%
- Witnessing war-related atrocities: 5.4%
- Unexpected death of a loved one: 5.4%
- Physical abuse during childhood: 5%
- Serious accidents (non-automobile)t: 4.9%
- Being a war refugee: 4.5%
- Combat experience: 3.6%
- Accidentally killing or injuring someone: 2.8%
- Automobile accident: 2.6%
- Physically assaulted: 2.5%
- Experiencing life-threatening illness: 2.0%
- Experiencing natural disaster: 0.3%
- PTSD in military veterans
Witnessing or taking part in war-related activities increases the risk of PTSD and other mental health conditions, such as substance use disorders.
PTSD in War Veterans
An estimated 354 million adult war survivors globally have PTSD and/or major depression. (European Journal of Psychotraumatology, 2019)
About 29% of living U.S. veterans who served in Iraq or Afghanistan have had PTSD. (National Center for PTSD, 2024)
About 21% of living U.S. veterans who served during the Persian Gulf War (Desert Storm) have had PTSD. (National Center for PTSD, 2024)
If you’d like to speak with someone from CRMC’s Behavioral Health team, call 218-545-1047 to schedule an appointment.
You Might Also Like
- CEO Amy Hart Recognized Nationally for Rural Health Excellence
- Heart Month: Know the Risks, Protect Your Heart, Save Lives
- Allina Health Minneapolis Heart Institute Offers Advanced Vascular Care at CRMC
- CRMC Upgrades MRI Technology for Faster, Clearer Scans
- Living With Incontinence? You’re Not Alone