Take back control.
Urology focuses on the treatment of disorders of the genito-urinary tract including kidneys, ureters, urinary bladder, urethra, and the male reproductive organs. Cuyuna Regional Medical Center Urology offers state-of-the-art care in the diagnosis, treatment, and management of both male and female urinary tract conditions and reproductive issues, including offering robotic-assisted surgery when indicated using the latest da Vinci Xi® robot.
CRMC recognizes the importance of providing individualized treatment plans that meet patients’ complex needs effectively. Our Urology division delivers care focused on clear communication, flexibility, and is grounded in years of experience, ensuring patients are provided with a comfortable and comprehensive experience. Care includes screening, diagnostic evaluation, the full spectrum of clinical urology, in-clinic procedures, and surgery including robotic-assisted surgery. Our Urology care team is led by Board-Certified Urologists Dr. Brandon P. Reynolds and Dr. Matt J. Watson and includes skilled caregivers at all levels and roles.
- Cancer of the prostate, kidneys, bladder and male reproductive organs
- Urinary retention
- Urethral strictures
- Urinary urgency and frequency
- Over-active bladder
- Interstitial cystitis
- Enlarged prostate or BPH
- Kidney stones
- Erectile dysfunction
- Chronic urinary tract infection
- Prostatitis/prostadynia
- Female and male urinary incontinence
- Genital disorders or conditions
- Hypogonadism or low testosterone in men
- Male reproductive issues
- Cancer screening
- Diagnostic evaluation and work-up or all urologic conditions
- In-office diagnostics such as Urodynamics, Uro-cuff, prostate biopsy, bladder ultrasound, PCR-based infection detection, the latest gene-based cancer diagnostic tests
- In-office procedures including, cystoscopy, vasectomy, minimally invasive prostate procedures, injections, cancer treatments, circumcision, meatotomy, bladder instillations, bladder botox injection, tibial nerve stimulation for OAB, Percutaneous stim trials for sacral neuromodulation
- Referral to appropriate affiliated providers including pelvic floor PT, biofeedback, counseling, gynecology
- Full spectrum of Genito-urinary surgical care
- Scrotal surgery including hydrocelectomy, spermatocelectomy
- Vasectomy
- ESWL (extracorporeal shockwave lithotripsy)
- Ureteroscopy with laser lithotripsy and stone extraction
- PCNL (percutaneous nephrolithotripsy)
- Robotic-assisted Partial Nephrectomy
- Laparoscopic Nephrectomy
- Robotic-Assisted Radical Prostatectomy
- Robotic-Assisted Pyeloplasty
- DVIU (direct vision internal urethrotomy)
- Circumcision
- Laparoscopic Varicocelectomy
- Interstim sacral neuromodulator implant
- Bladder Botox injection
- TURBT (resection of bladder tumors)
- Hydrodistension
- Cystolitholapaxy
- Repair vesico-vaginal fistula
- Bladder diverticulectomy
- Partial cystectomy
- Green Light Laser Vaporization of the Prostate
- Transurethral resection of the prostate (TURP)
What is BPH?
Benign Prostatic Hyperplasia, or BPH, is a condition in which the prostate enlarges as men get older. BPH is a very common condition that affects over 40 million Americans and over 500 million aging men worldwide. Over 40% of men in their 50s and over 70% of men in their 60s have BPH. While BPH is a benign condition and unrelated to prostate cancer, it can greatly affect a man’s quality of life.
As the prostate enlarges, it presses on and blocks the urethra, causing bothersome urinary symptoms such as:
- Frequent need to urinate both day and night
- Weak or slow urinary stream
- A sense that you cannot completely empty your bladder
- Difficulty or delay in starting urination
- Urgent feeling of needing to urinate
- A urinary stream that stops and starts
If you suffer from the above symptoms, you are not alone. BPH is the leading reason men visit a urologist. You can measure the severity of your BPH symptoms by taking the International Prostate Symptom Score (IPSS) questionnaire.
What is the UroLift System?
Treatment with the UroLift® System uses a minimally invasive approach that provides rapid relief and recovery of BPH symptoms. It is an earlier treatment option that can get men off BPH medications and avoid major surgery. The goal of the UroLift System treatment is to relieve symptoms so you can get back to your life and resume your daily activities.
The UroLift® System treatment has demonstrated a significant improvement in quality of life for patients that is greater than reported for medications. The UroLift® System is the only BPH procedure shown not to cause new and lasting erectile or ejaculatory dysfunction, while being a safe and effective treatment of lower urinary tract symptoms due to BPH.
How Does The UroLift® System Work?
The UroLift® System uses a revolutionary approach to treating BPH that lifts and holds the enlarged prostate tissue so it no longer blocks the urethra. It is the only available BPH treatment performed by a urologist that does not require heating, cutting, or removal of the prostate tissue. The procedure is typically performed using local anesthesia in a physician’s office or ambulatory surgery center. Patients typically return home the same day without a catheter.
Frequently Asked Questions
Who is a good candidate for the UroLift® System treatment? You may be a good candidate if you are a male, 45 years of age or older, and have symptoms relating to BPH. Speak with your urologist to see if the UroLift® System treatment is right for you. If you have a known allergy to nickel, titanium or stainless steel, talk to your doctor about your allergy before getting a UroLift System treatment.
What should I expect during the treatment? Is it painful? How long does it take? If you and your doctor decide that the UroLift® System treatment is right for you, your doctor will provide you with more detailed information relating to the treatment. In general, the UroLift System is a minimally invasive treatment that entails minimal downtime. Your doctor will use the UroLift Delivery Device to deploy permanent implants to relieve obstruction caused by the enlarged prostate that is pressing on your urethra. The procedure, which usually takes about an hour, may be performed under local or general anesthesia and you may be given medication to feel comfortable during the treatment. This typically helps minimize discomfort during the procedure, though everyone’s definition for pain and discomfort varies greatly. Typically, no catheter and no overnight stay is required post-treatment.
What happens post-treatment, during the recovery period? Are meds required? After the treatment, patients typically go home the same day without a catheter. There is minimal downtime posttreatment and many patients experience symptom relief in as early as 2 weeks. Patients may experience some urinary discomfort during the recovery period. Most common side effects are mild to moderate and include pain or burning with urination, blood in the urine, pelvic pain, urgent need to urinate and/or the inability to control the urge. Most symptoms resolved within two to four weeks after the procedure.
Does the treatment affect my sexual function? Clinical studies have shown the UroLift® System treatment does not cause new, sustained instances of erectile or ejaculatory dysfunction. The same cannot always be said of other BPH therapies such as TURP, laser, and even medication.
Does my insurance cover the treatment? The UroLift® System treatment is covered by Medicare and all major private insurers. Contact your insurance provider for your specific coverage information.
Talking to Your Doctor about BPH
BPH is a very common condition and is one of the leading reasons men visit a urologist. Whether you have just started experiencing symptoms or if you've tried various medications or even surgery, there are a range of treatment options available.
Before you visit the doctor's office, you can take this BPH Symptom Quiz, designed by the American Urological Association, to determine the severity of your symptoms. We will discuss your symptoms together to decide which treatment option is best for you. Schedule an appointment today to discuss your BPH symptoms with us.

GreenLightTM Laser Therapy
Advanced treatment for benign prostatic hyperplasia
Patient Information

Table of contents
- Introduction
- What is GreenLight™ Laser Therapy?
- When medicine isn’t enough – alternative treatment options
- Advantages of GreenLight Laser Therapy
- What happens during the GreenLight procedure?
- After the procedure
- Risks
- Tried and tested technology
- Next steps
- Frequently asked questions
- Resources
- Commonly used terms
- References
If you have been diagnosed with an enlarged prostate and medications are not working, it may be time to consider another option.
Talk to your doctor about GreenLight™ Laser Therapy
Introduction
You are receiving this brochure because you have been diagnosed with benign prostatic hyperplasia (BPH), commonly known as an enlarged prostate and may be a candidate for GreenLight Laser Therapy.
An enlarged prostate can mean frequent trips to the bathroom and interrupted sleep. Medicines for this condition may not work that well, can be expensive and may have unpleasant side effects.
If this sounds like you, it’s time to take action. There are more treatment options today than ever before.
GreenLight Laser Therapy has helped hundreds of thousands of men similar to you gain relief from frustrating BPH symptoms affecting their lives and the people closest to them.
We hope you find this brochure informative and that it helps you find the right treatment option for your condition. If you have additional questions, please be sure to ask your doctor.
With GreenLight Laser Therapy, you can get help with your BPH symptoms, to help you quickly get back to the things you like to do.
What is GreenLightTM Laser Therapy?
GreenLight Laser Therapy has helped over 900,000 men worldwide.1
Lasers are now used in many areas of medicine, including eye2 and cosmetic surgery.3 They are also used to treat an enlarged prostate.4
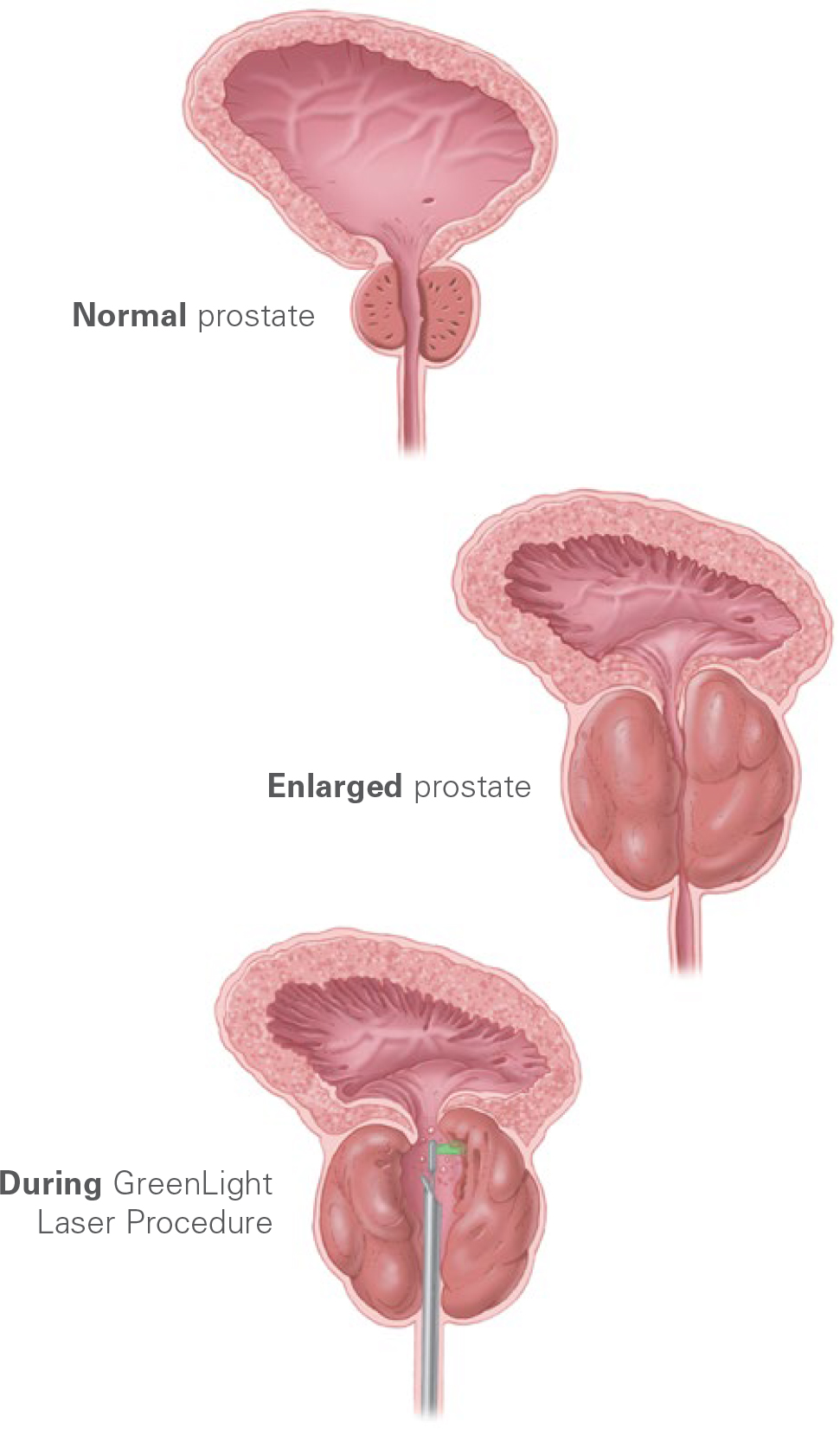
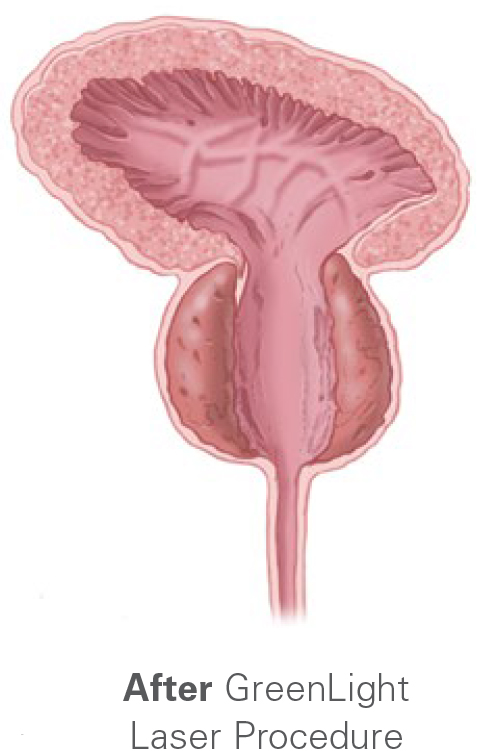
During the GreenLight procedure, the tissue blocking your prostate is rapidly heated and vaporized. Natural urine flow is rapidly restored in most patients.
Typically, the procedure is performed as a same-day surgery. Many patients can go home without a urinary catheter. An overnight stay may be recommended for some patients.
When medicine isn’t enough
Alternative treatment options
Typically, medicines are first used to treat an enlarged prostate. However, sometimes drugs don’t provide enough symptom relief. Or the side effects can be bothersome. Drugs can be expensive. Or there may be other reasons medical therapy for BPH isn’t right for you.
Fortunately, there are alternatives. Surgical methods to treat an enlarged prostate include:
Transurethral resection of the prostate (TURP) – This procedure involves use of a heated wire to cut tissue from the prostate and has been used to treat an enlarged prostate for years.
Open surgery – This procedure involves removal of the inner part of the prostate through an incision made in the abdomen.
Other types of lasers – In addition to GreenLight Laser Therapy, other systems remove enlarged prostate tissue through the use of high-energy lasers. Clinically documented laser therapies have become a viable treatment option.5
Transurethral microwave therapy (TUMT) – In this therapy, a microwave antennae mounted on a catheter is used to heat the prostate and open up the blockage.
GreenLight™ Laser Therapy Redefining the standard of care for an enlarged prostate

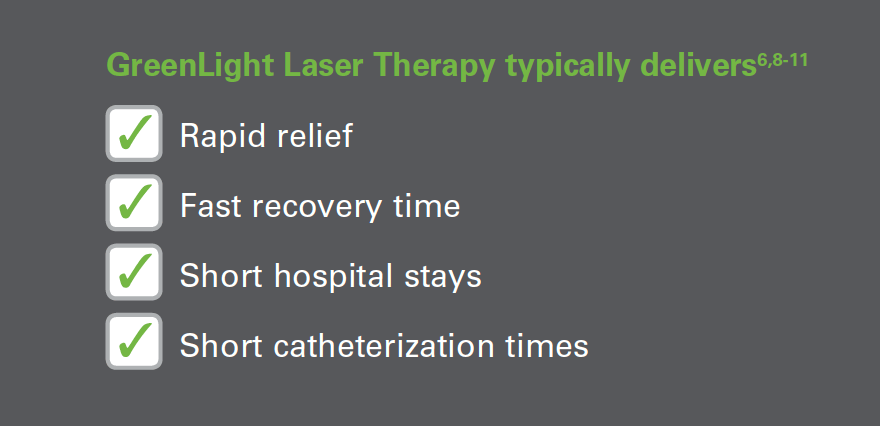
Advantages of GreenLight Laser Therapy
Compared with traditional surgical options, GreenLight Laser Therapy is associated with:
- Significantly less chance of severe blood loss6
- Same-day surgery in most cases7
- Significantly faster recovery in typical cases for the following:6,8-11
- Shorter hospital stay
- Shorter catheterization time
- Less bleeding
- Comparable risks and outcomes
Hospital length of stay and time with a urinary catheter are typically shorter with the GreenLight procedure than TURP.6,8-11
What happens during the GreenLightTM procedure?
The following is intended as a general overview. Your experience may differ. Please talk to your doctor about potential risks and questions you may have about the procedure.
- Before treatment begins, you may be asked to empty your bladder.
- You will then be brought into the procedure room and moved to the treatment bed where you will lie on your back. Your doctor may give you medication to help you relax.
- The procedure is typically performed under general anesthesia. This means that you will be asleep during the procedure. A different type of anesthesia may be used, depending on the treatment center.
- Once the anesthesia takes effect, your doctor will insert a small scope into your urethra. The scope allows your doctor to see the inner surfaces of the urethra, prostate and bladder.
- After the scope is in place, your doctor will advance the laser device through the scope to the location of the enlarged prostate tissue.
- Your doctor will then vaporize the prostate tissue that is obstructing urine flow. Dead tissue that is not immediately vaporized will be passed naturally in your urine during the first few days after your surgery.
- A temporary urinary catheter may be placed at the end of the procedure to let urine drain from your bladder.
After the procedure
People typically go home within a few hours after the procedure. You should arrange for a ride home.
If a urinary catheter was placed in your bladder at the end of the procedure, it will typically be removed within 24 hours. However, some patients may require a catheter for a longer time.
Most patients experience very rapid relief of symptoms and a dramatic improvement in urine flow. This usually occurs within 24 hours of the procedure. Your experience may differ. Your doctor will provide you with specific discharge instructions and information on signs and symptoms that may require further medical attention.
You may experience mild discomfort such as slight burning during urination and see small amounts of blood in your urine for a week or so. Also, depending on the condition of your bladder, you may experience greater frequency and urge to urinate. This will likely resolve over time.
Usually, you can return to your everyday activities within a short time after the GreenLight procedure. If you have any questions, ask your doctor.
Risks
Every surgical procedure may have risks. The same is true for GreenLight™ Laser Therapy.
The most common risks include:
- Hematuria – Blood in the urine
- Irritation of the bladder – Results in frequent and/or urgent need to urinate
- Irritation of the urethra – Frequent urination, burning sensation
- Retrograde ejaculation – Semen during sexual climax travels backward to the bladder rather than exiting through the penis
At doctor’s instruction, some patients taking blood-thinners can be treated with GreenLight Laser Therapy without stopping their medicines.12
Tried and tested technology
GreenLight™ Laser Therapy has been well documented and numerous articles have been published about the therapy in medical literature.
Based on these articles, GreenLight Laser Therapy:
- Has low complication rates6, and short catheterization6,8-11,13-14 and hospitalization times.6,8-11,14
- Can be used if you are taking blood thinners12, in urinary retention15, or have a large prostate (>100 ml).8
- Can be used if you have an implanted pacemaker, defibrillator, or neurostimulator.16

Next steps
You can get back to your life without the hassles of remembering to take BPH or enlarged prostate pills, dealing with side effects, and paying for prescriptions.
Talk to your doctor to see if GreenLight Laser Therapy is right for you.
It just might be the best choice for symptom relief from an enlarged prostate. It’s time to take action and get measurable results – without medications.
Frequently asked questions
Q. Is prostate enlargement a type of cancer?
A. No. Prostate enlargement occurs naturally as a man ages. It will affect approximately 50 percent of men between the ages of 51 and 60 and up to 90 percent of men over the age of 80.17 No one knows exactly why the condition occurs.
Q. Do I have to stay in the hospital after a GreenLight™ procedure?
A. GreenLight Laser Therapy is generally performed as a same-day surgical procedure. Typically, an overnight stay in the hospital is not required.
Q. What effect does the GreenLight procedure have on sexual function?
A. In a recent study, 86% of patients reported improved or unchanged sexual satisfaction; 14% worsened. Similar outcomes were seen for erectile function.8
Q. How long does it take until symptoms are relieved?
A. Most patients experience very rapid relief of symptoms and improvement in urine flow within 24 hours of the procedure. However, medical history, health conditions, and other factors can influence treatment and recovery.
Q. Will I continue to need prostate medication after the GreenLight procedure?
A. Most patients are able to discontinue taking their prostate medication within a few weeks after the GreenLight procedure. However, as with any medication, consult with your doctor before making any changes to your dosing.
Q. How soon can I return to work?
A. Most patients can resume their normal activities within a couple of days. Strenuous activities can be resumed within a short time. Your doctor will discuss any restrictions and your specific condition with you during your visit following your procedure.
Q. Is GreenLight Laser Therapy covered by insurance?
A. Yes, GreenLight Laser Therapy is covered by Medicare and most private insurers.
Boston Scientific does not guarantee insurance coverage for any procedure or product. It is the responsibility of the patient to contact their insurance provider for specific coverage information.
Resources
We understand how important it is to get answers to questions that you might have about prostate health. The following resources can help you learn more about advances in the diagnosis and treatment of an enlarged prostate.

GreenLight™ Laser Therapy patient website – You can find a wealth of information about GreenLight Laser Therapy on our website at:
- Take a quiz to gauge the degree of your condition
- Find a local urologist
- Learn more about BPH and find additional educational resources
Urology Care Foundation – The Urology Care Foundation is the official foundation of the American Urological Association and provides extensive information on prostate health on its website at:
National Kidney and Urologic Diseases Information Clearinghouse (NKUDIC) – This website is sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health (NIH). In addition to basic information on an enlarged prostate, you will find links to the latest research and statistics on prostate health at:
Commonly used terms
Benign prostatic hyperplasia (BPH): A non-cancerous enlargement of the prostate.
Bladder: Hollow organ in the lower abdomen that stores urine.
Catheter: A flexible tube for withdrawing fluids from (or introducing fluids into) a cavity of the body, especially for inserting into the bladder, through the urethra, to remove urine.
Ejaculation: The release of semen from the male reproductive system. Erectile dysfunction: Inability to develop or maintain an erection.
Hematuria: Blood in the urine.
Impotence: Inability to maintain an erection and/or the inability to ejaculate.
Incontinence: Loss of control of the bladder. Can range from minor leakage to total inability to control bladder function.
Laser energy: A highly concentrated, very intense beam of light energy that can create high temperatures.
Prostate: Gland in males located in front of the rectum and below the bladder. The main function of the prostate is to transport sperm during ejaculation.
Retrograde ejaculation: Semen travels backward to the bladder during sexual climax rather than exiting through the penis.
TUMT: Treatment for an enlarged prostate that uses heat to treat an enlarged prostate. Stands for transurethral microwave therapy.
TURP: Common surgical treatment for an enlarged prostate. Stands for transurethral resection of the prostate.
Urethra: Tube that connects the urinary bladder to the genitals for the removal of fluids from the body.
Urinary urgency: A sudden, compelling urge to urinate.
References
- Data on file with Boston Scientific.
- Munnerlyn CR. Lasers in ophthalmology: Past, present and future. J Mod Opt. 2003;50:2351-60.
- Hruza GJ, Dover JS. Laser skin resurfacing. Arch Dermatol. 1996 Apr;132(4):451-5.
- McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011 May;185(5):1793-803.
- Hueber PA, Zorn KC. Canadian trend in surgical management of benign prostatic hyperplasia and laser therapy from 2007-2008 to 2011-2012. Can Urol Assoc J. 2013 Sep-Oct;7(9-10):E582-6.
- Bachmann A, Tubaro A, Barber N, et al. 180-W XPS GreenLight laser vaporization versus transurethral resection of the prostate for the treatment of benign prostatic obstruction: 6 month safety and efficacy results of the European multi-centre randomized trial – The GOLIATH Study. Eur Urol. 2014 May;65(5):931-42.
- Garnick MB. 2013 Annual Report on Prostate Diseases. Boston, MA: Harvard Health Publications; 2013.
- Lukacs B, Loeffler J, Bruyère F, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: A multicenter randomized controlled trial. Eur Urol. 2012 Jun;61(6):1165-73.
- Capitán C, Blázquez C, Martin MD, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: A randomized clinical trial with 2-year follow-up. Eur Urol. 2011 Oct;60(4):734-9.
- Al-Ansari A, Younes N, Sampige VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol. 2010 Sep;58(3):349-55.
- Bouchier-Hayes DM, Van Appledorn S, Bugeja P, et al. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium titanylphosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int. 2010 Apr;105(7):964-9.
- Sohn JH, Choi YS, Kim SJ, Effectiveness and safety of photoselective vaporization of the prostate with the 120 W HPS GreenLight laser in benign prostatic hyperplasia patients taking oral anticoagulants. Korean J Urol. 2011 Mar;52(3):178-83.
- Ahyai SA, Gilling P, Kaplan SA, et al. Meta-analysis of functional outcomes and complications following transurethral procedures for lower urinary tract symptoms resulting from benign prostatic enlargement. Eur Urol. 2010 Sep;58(3):384-97.
- Pereira-Correia JA, de Moraes Sousa KD, Santos JB, et al. GreenLight HPS™ 120-W laser vaporization vs transurethral resection of the prostate (<60 mL): A 2-year randomized double-blind prospective urodynamic investigation. BJU Int. 2012 Oct;110(8):1184-9.
- Woo H, Reich O, Bachmann A, et al. Outcome of GreenLight HPS 120W laser therapy in specific patient populations: those in retention, on anticoagulants, and with large prostates (≥ 80 ml). Eur Urol. 2008;7(Suppl):378-83.
- GreenLight XPS™ Laser System Operator’s Manual, Part No. 0010- 0240 Rev. C. November 2010.
- Barry M, Roehrborn C. Management of benign prostatic hyperplasia. Ann Rev Med. 1997 Feb;48:177-189.
All surgical treatments have inherent and associated risks. The GreenLight™ Laser System is intended for removal of soft tissue, including vaporization of the prostate for benign prostatic hyperplasia (BPH). Potential risks include irritative symptoms, bleeding, retrograde ejaculation and urinary tract infection. You should talk with your doctor about benefits and risks before moving forward with any treatment option.
CAUTION: U.S. Federal law restricts this device to sale by or on the order of a physician.
CAUTION: The law restricts this device to sale by or on the order of a physician. Indications, contraindications, warnings and instructions for use can be found in the product labelling supplied with each device. Information for use only in countries with applicable health authority registrations. Material not intended for use in France.
All trademarks are the property of their respective owners.

![]()
Make space for life as usual
Minimizing potential side effects of prostate cancer radiation therapy
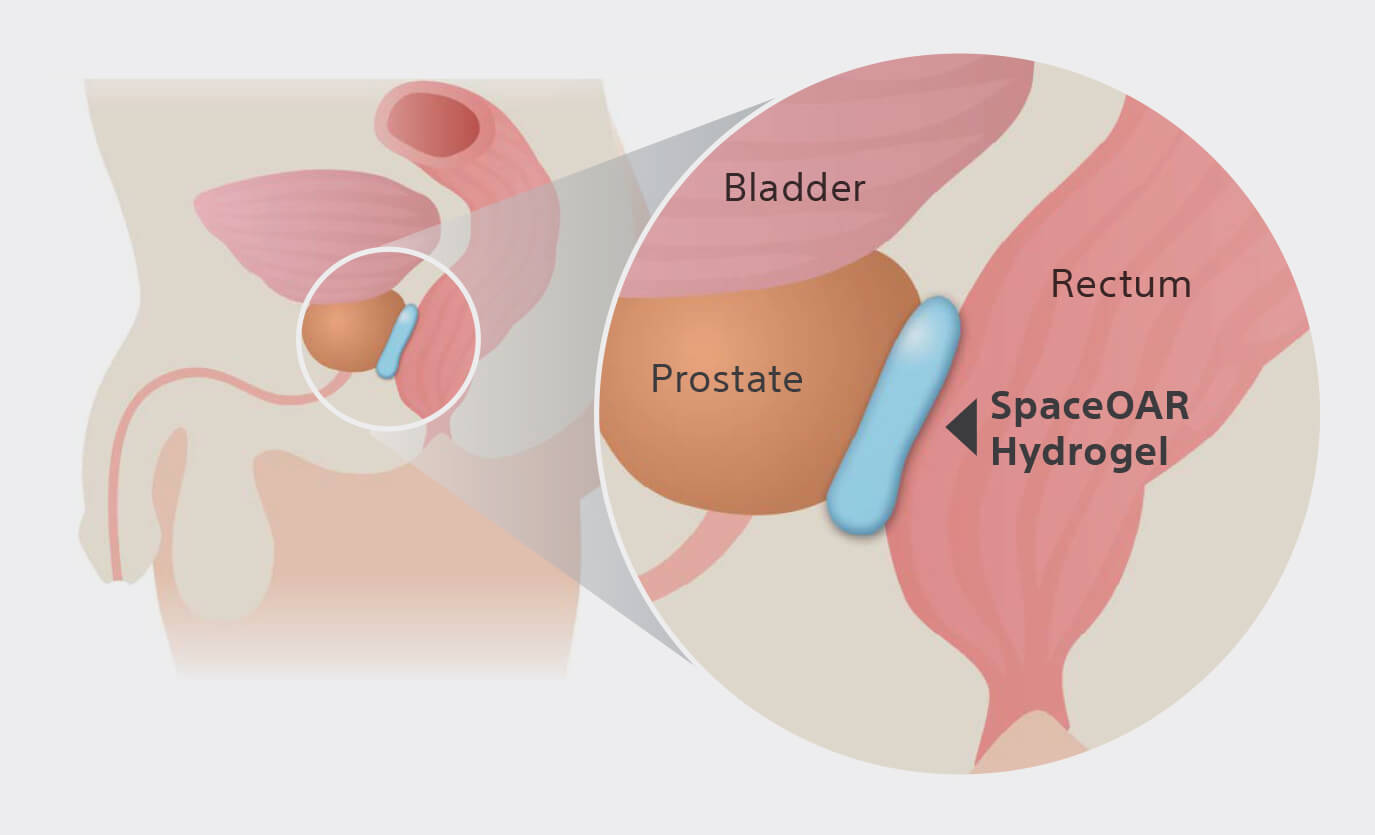
SpaceOAR Hydrogel is an absorbable PEG-based hydrogel that temporarily creates space between the prostate and rectum, designed to reduce radiation dose to the rectum to help minimize the side effects of radiation therapy.1
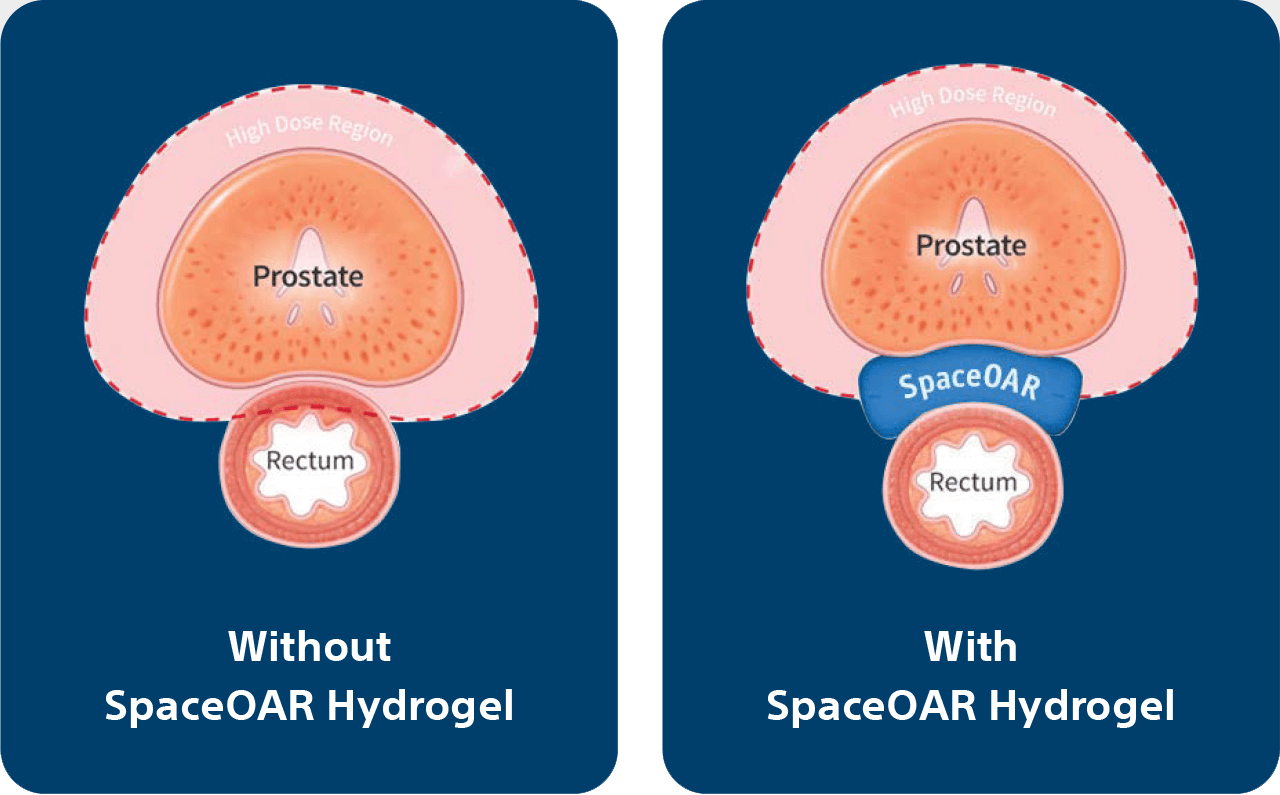
Radiation therapy can be extremely effective in treating prostate cancer, but as with any procedure, there are potential side effects. The prostate is next to the rectum. Due to the proximity, prostate radiation therapy can unintentionally cause damage to the rectum, which can lead to issues with bowel function.2
SpaceOAR Hydrogel is designed to temporarily create space between the prostate and the rectum, reducing the radiation dose delivered to the rectum during prostate radiation therapy which may lessen damage to the rectum.3,4
More space can mean better quality of life.
- Fewer long-term side effects3,4
- More likely to report maintenance of sexual function5
- Significantly lower decline in urinary and bowel function3,4
To learn about SpaceOAR Hydrogel or to connect to more resources, visit spaceoar.com
Frequently Asked Questions
What is it made of?
SpaceOAR Hydrogel is a soft gel material that is mostly made of water and polyethylene glycol (PEG), which is commonly used in other medical implants. The material is biodegradable and is designed to be absorbed and leave your body naturally after about 6 months.1
Where is the procedure performed?
The procedure to implant SpaceOAR Hydrogel is generally a brief outpatient procedure, and can be done in a doctor’s office, hospital or clinic before starting radiation treatment.1
Is SpaceOAR Hydrogel widely used?
SpaceOAR Hydrogel is now the option of choice for doctors and patients prior to radiation therapy. It is used in leading cancer centers, and with most types of radiation therapy. Many radiation oncologists, urologists and interventional radiologists recommend SpaceOAR Hydrogel for their prostate cancer patients.1
Read more on spaceoar.com/faqs
“Once I learned more about SpaceOAR Hydrogel, there was no way I was going to get radiation therapy without it.”
– Pierre, Plano, TX | SpaceOAR Hydrogel patient
Hear from other patients.
Scan the QR code with your phone camera or visit spaceoar.com/spaceoar-patient-testimonials
- Open your phone’s camera app
- Point the camera at the QR code square and your phone will recognize the code
- Tap the alert at the top of your screen to visit the website
This guide is informational and not intended to be a substitute for a thorough discussion with your doctor.
REFERENCES & DISCLAIMERS
- Data on file with Boston Scientific.
- American Cancer Society. Radiation Therapy for Prostate Cancer. Accessed September 9, 2021. https://www.cancer.org/cancer/prostate-cancer/treating/radiation-therapy.html
- Mariados N, Sylvester J, Shah D, et al. Hydrogel spacer prospective multicenter randomized controlled pivotal trial: Dosimetric and clinical effects of perirectal spacer application in men undergoing prostate image guided intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys. 2015 Aug 1;92(5):971-7.
- Hamstra DA, Mariados N, Sylvester J, et al. Continued benefit to rectal separation for prostate radiation therapy: Final results of a phase III trial. Int J Radiat Oncol Biol Phys. 2017 Apr 1;97(5):976-85.
- Hamstra DA, Mariados N, Sylvester J, et al. Sexual quality of life following prostate intensity modulated radiation therapy (IMRT) with a rectal/prostate spacer: Secondary analysis of a phase 3 trial. Pract Radiat Oncol. 2018 Jan - Feb;8(1):e7-e15.
SpaceOAR Hydrogel contains Polyethylene Glycol (PEG).
As with any medical treatment, there are some risks involved with the use of SpaceOAR Hydrogel. Potential complications associated with SpaceOAR Hydrogel include, but are not limited to: pain associated with SpaceOAR Hydrogel injection, pain or discomfort associated with SpaceOAR Hydrogel, local inflammatory reactions, infection (including abscess), urinary retention, urgency, constipation (acute, chronic, or secondary to outlet perforation), rectal tenesmus/muscle spasm, mucosal damage, ulcers, fistula, perforation (including prostate, bladder, urethra, rectum), necrosis, allergic reaction (localized or more severe reaction, such as anaphylaxis) embolism (venous or arterial embolism is possible and may present outside of the pelvis, potentially impacting vital organs or extremities), syncope and bleeding. The occurrence of one or more of these complications may require treatment or surgical intervention. Please talk to your doctor about the risks and benefits associated with SpaceOAR Hydrogel.
Results from case studies are not necessarily predictive of results in other cases. Results in other cases may vary. Content of this brochure is for Information Purposes only and does not constitute medical advice. Boston Scientific strongly recommends that you consult with your physician on all matters pertaining to your health or to address any questions.
CAUTION: U.S. Federal law restricts this device to sale by or on the order of a physician.
CAUTION: The law restricts these devices to sale by or on the order of a physician. Indications, contraindications, warnings and instructions for use can be found in the product labeling supplied with each device. Information for use only in countries with applicable health authority registrations. This material not intended for use in France.
Products shown for INFORMATION purposes only and may not be approved or for sale in certain countries. Please check availability with your local sales representative or customer service. All images are the property of Boston Scientific. All trademarks are the property of their respective owners.
©2022 Boston Scientific Corporation or its affiliates. All rights reserved. UROPH-623715-AC APR 2022
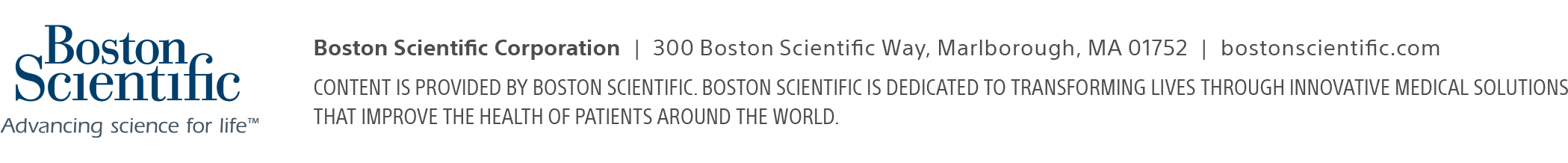
Evidence suggests that breakdowns in the bladder-brain communication pathway may be a root cause of OAB and non-obstructive urinary retention.1,2,3 That’s why conventional treatments may not produce the results you want – they don’t directly target this miscommunication. Unlike conventional treatments, the Medtronic InterStim systems gently stimulate the sacral nerves in the pelvic area that control the bladder.4,5 This may help restore* bladder-brain communication and reduce symptoms.
Get more control with the InterStim Systems6,7
- 84% satisfaction among those who use it8
- 3X greater improvements in OAB quality of life9
- 82% of people achieved success† at 5 years6
- Only therapy that lets you see if it works before you and your doctor decide
- More than 375,000 people worldwide have chosen the Medtronic InterStim systems for more control and long-lasting relief6,7
- Recharge-free and rechargeable options let you choose the right device for your lifestyle
In addition to risks related to surgery, complications can include pain at the implant sites, new pain, infection, lead (thin wire) movement/migration, device problems, undesirable changes in urinary or bowel function, and uncomfortable stimulation (sometimes described as a jolting or shocking feeling). Talk with your doctor about ways to minimize these risks.

Is InterStim Right for You?
You may be a good candidate for Medtronic Bladder Control Therapy delivered by the InterStim systems if:
- You have significant OAB symptoms or non-obstructive urinary retention
- You’ve tried lifestyle changes and oral medications
- These therapies haven’t given you the relief you want
Say yes to the test
Take back control with an evaluation for an InterStim system
Unlike other bladder control treatments, this therapy lets you try it first with an evaluation – like a test run, not a long-term commitment.
Here’s how it works:
- The simple test starts at your doctor’s office or an outpatient center.
- A lead (thin wire) is inserted in the upper part of your buttock.
- The lead attaches to a small external device worn discreetly under your clothes.
- Stop, start, or adjust the therapy settings, with an easy-to-use programmer that resembles a smartphone.
- Go about most of your regular activities for 3 to 14 days
- Track your symptoms to see if they improve
Complications can occur with the evaluation, including movement of the wire, technical problems with the device, and some temporary pain. Your doctor or nurse will show you how to use the system and inform you of any activity restrictions and other precautions related to the evaluation.
Get more personalized treatment options
After your test, talk to your doctor about the results. Together, you can choose a powerful and personalized solution for your long-term care. Your evaluation device can be replaced with an implantable device called a neurostimulator during a short, outpatient procedure.
Bladder control therapy has risks similar to any surgical procedure. The most common adverse events experienced during clinical studies include pain at implant sites, new pain, lead migration, infection, technical or device problems, adverse change in bowel or voiding function, and undesirable stimulation or sensations. Any of these may require additional surgery or cause return of symptoms. Discuss these potential risks and benefits with your doctor.
More control starts with our smart programmer
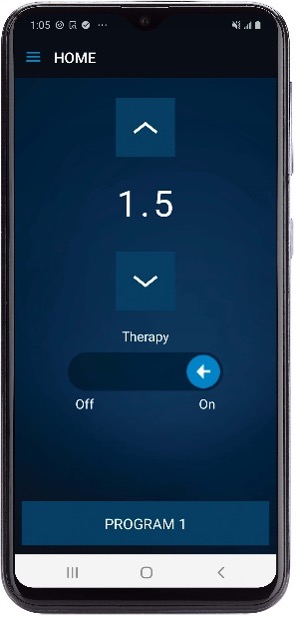
The smart programmer allows you and your healthcare provider to manage your therapy as needed. Unlike previous iterations of our technology that resembled a key fob without a display screen, our Smart Programmer allows you:
- Visibility to check your stimulation level on a clear, easy-to-read screen
- Adjust your stimulation with confidence that its been changed to the setting you intended
- Turn stimulation on or off
- Change therapy programs (as directed by your healthcare provider)
- Activate MRI mode and check MRI eligibility (see more information below)
MRI Confidence
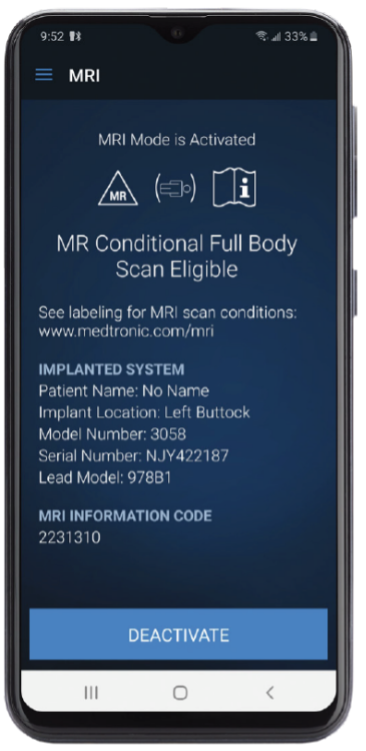
Medtronic’s proprietary SureScan™ MRI technology is what enables patients to get full-body‡ 1.5 and 3T MRI scans. It is the only sacral neuromodulation system with this SureScan technology. This means:
- Full-body‡ 1.5 and 3T scans
- No impedance checks required prior to MRI scans
- Scans allowed even if you have had out-of-range impedances
- MRI mode is easy to activate or deactivate on Medtronic’s smart programmer without clinician or Medtronic interaction
- Digital display for clear confirmation of MRI mode activation
Access the Medtronic InterStim MRI Brochure to learn about our MRI Center of Excellence and MRI testing lab and for information on how to activate MRI mode on your smart programmer.
*Restored function defined as a 50% or greater reduction in dysfunctional voiding symptoms from baseline
†Numbers reflect completers analysis defined as patients with diary data at baseline and 12 months (n=220). Clinical success was 82% at 12 months using the modified completers analysis (subjects who either had a baseline and 12-month evaluation or withdrew early due to device-related reasons and are considered failures). Success defined as a 50% or greater reduction in your troublesome bladder symptoms.
‡Under certain conditions; see approved labeling for details. Patients with InterStim™ SureScan™ MRI Leads only.
1. Dasgupta R. Critchley HD, Dolan RJ, Fowler CJ. Changes in brain activity following sacral neuromodulation for urinary retention. J Urol. 2005; 174:2268-2272
2. Griffiths D, Derbyshire S, Stenger A, Resnick N. Brain control of normal and overactive bladder. J Urol. 2005; 174:1862-1867.
3. Griffiths D, Tadic SD. Bladder control, urgency, and urge incontinence: evidence from functional brain imaging. Neurourol Urodyn. 2008;27(6):466-474.
4. Kenefick NJ, Emmanuel A, Nicholls RJ. Effect of sacral nerve stimulation on autonomic nerve function. British Journal of Surgery. 2003;90:1256-1260.
5. Patton V, Wiklendt L, Arkwright JW, Lubowski DZ, Dinning PG. The effect of sacral nerve stimulation on distal colonic motility in patients with fecal incontinence. Br J Surg. 2013;100:959-968.
6. Siegel S, Noblett K, Mangel J, et al. Five-year follow-up results of a prospective, multicenter study of patients with overactive bladder treated with sacral neuromodulation. J Urol. 2018; 199(1), 229-236.
7. Medtronic InterStim Therapy Clinical Summary (2018).
8. Foster RT Sr, Anoia EJ, Webster GD, Amundsen CL. In patients undergoing neuromodulation for intractable urge incontinence a reduction in 24-hr pad weight after the initial test stimulation best predicts long-term patient satisfaction. Neurourol Urodyn. 2007; 26:213-217.
9. Siegel S, Noblett K, Mangel J, et al. Results of a prospective, randomized, multicenter study evaluating sacral neuromodulation with InterStim® Therapy compared to standard medical therapy at 6-months in subjects with mild symptoms of overactive bladder. Neurourol Urodyn. 2015; 34:224-230.
Frequently Asked Questions
Why is this therapy different?
You can try it before you decide, and it’s reversible if you change your mind later. And unlike injections, it doesn’t require self-catheterization or repeated treatment visits.
What can this therapy do for me?
It may significantly reduce symptoms in people who have frequent urges to urinate or related frequent leaks or are unable to fully empty their bladder.1
Will it cure my condition?
No. It can be effective, but it’s not a cure. If the neurostimulator is turned off or removed, symptoms can return.
What does the stimulation feel like?
Most people describe the stimulation sensation as a tingling, flutter, or vibration in the pelvic area. It should not be painful. Stimulation settings can be adjusted, and sensations will vary from person to person.
Can I have an MRI?
People with an InterStim™ system can have a full-body‡ MRI scan under certain conditions. Your doctor will determine whether you meet those conditions.
Will insurance cover the costs?
Medicare and many private insurance companies cover this therapy. Talk to your doctor to learn more about your insurance coverage.
6. Foster RT Sr, Anoia EJ, Webster GD, Amundsen CL. In patients undergoing neuromodulation for intractable urge incontinence a reduction in 24-hr pad weight after the initial test stimulation best predicts long-term patient satisfaction. Neurourol Urodyn. 2007; 26:213-217
Resources
Record your symptoms to help your doctor understand your condition.
Care Pathway for Bladder Control
Understand all of your treatment options for dealing with bladder control issues.
Starting the conversation can be hard. This guide can help you talk to your doctor.
Medtronic Bladder Control Therapies
Understand your options and decide if a Medtronic Bladder Control Therapy is right for you.
Patient Therapy Guide – iCon™ Programmer (.pdf)
A handy guide to living with Medtronic Bladder Control Therapy delivered by the InterStim system, and to using your hand-held Medtronic iCon programmer.
Patient Therapy Guide – Smart Programmer (.pdf)
A handy guide to living with Medtronic Bladder Control Therapy delivered by the InterStim system, and to using your Samsung smart programmer device.